Components of a Diabetic Eye Exam
Pupil Dilation
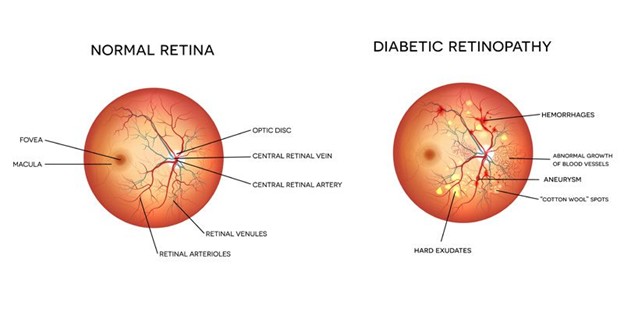
Though optional, we highly recommend it for diabetics. It lets us see the furthest corners of the retina, where dangerous signs like neovascularization or retinal detachment might be hiding.
Optical Coherence Tomography (OCT)
Eye Pressure Check
Optos Ultra Widefield Retinal Imaging
Retinal Photography
High-resolution images of the macula and optic nerve, the most vision-critical parts of the eye. These photos are stored digitally to monitor change over time and help detect swelling or degeneration.
How Often Should Diabetics Have Eye Exams?
- Type 1 Diabetes: Start 5 years after diagnosis, then every year
- Type 2 Diabetes: Start at diagnosis, then every year
- More frequent exams may be recommended if complications arise
